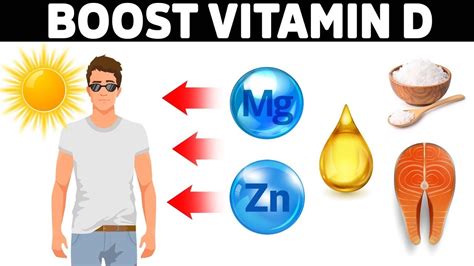
Optimal vitamin D absorption may hinge on timing, with experts suggesting that taking the supplement alongside the largest meal of the day can significantly boost its effectiveness. Studies indicate that taking vitamin D with food, particularly a meal containing fats, enhances absorption compared to taking it on an empty stomach.
Vitamin D Absorption: Maximizing the Benefits Through Strategic Timing
Experts are emphasizing the importance of timing when it comes to vitamin D supplementation, pointing to research that suggests taking the nutrient with the largest meal of the day can substantially increase its absorption. Vitamin D, a fat-soluble vitamin, requires the presence of dietary fats to be effectively absorbed in the digestive system. Consequently, the timing of vitamin D intake relative to food consumption plays a critical role in optimizing its bioavailability.
According to Dr. Carol Haggans, a registered dietitian and consultant to the National Institutes of Health, “Vitamin D is a fat-soluble vitamin, so it is best absorbed when taken with a meal containing fat.” This underscores the importance of pairing vitamin D supplements with food to maximize its absorption.
Studies have consistently demonstrated the superior absorption of vitamin D when consumed with meals containing fats. A study published in the Journal of the Academy of Nutrition and Dietetics found that vitamin D absorption was significantly greater when taken with a meal containing fat compared to a fat-free meal. The research showed a 32% increase in vitamin D absorption when it was taken with a fat-containing meal.
The Science Behind Fat-Soluble Vitamin Absorption
Understanding the physiology of fat-soluble vitamin absorption is essential to appreciate the significance of timing. Fat-soluble vitamins, including vitamins A, D, E, and K, are absorbed in the small intestine along with dietary fats. This process involves the formation of micelles, tiny spherical complexes that emulsify fats and fat-soluble vitamins, allowing them to be transported across the intestinal lining into the bloodstream.
When dietary fat is present, the body releases bile from the gallbladder, which aids in the emulsification and digestion of fats. Bile salts surround the fat molecules, breaking them down into smaller droplets and forming micelles. These micelles transport the fat-soluble vitamins to the surface of the intestinal cells, where they are absorbed. Without adequate dietary fat, the formation of micelles is compromised, and the absorption of fat-soluble vitamins, including vitamin D, is significantly reduced.
Practical Implications: Integrating Vitamin D Supplementation into Daily Routines
Given the importance of dietary fat for vitamin D absorption, individuals taking vitamin D supplements should strategically plan their intake to coincide with their largest, most fat-containing meal. This might be lunch or dinner, depending on individual dietary habits. The composition of the meal is also crucial. Meals rich in healthy fats, such as those containing avocado, nuts, seeds, olive oil, or fatty fish, are particularly effective at enhancing vitamin D absorption.
For individuals following low-fat diets, it may be necessary to make conscious efforts to include sources of healthy fats when taking vitamin D supplements. Even a small amount of fat, such as a tablespoon of olive oil or a handful of almonds, can significantly improve absorption.
It’s also important to consider the type of vitamin D supplement being taken. Vitamin D supplements are available in two primary forms: vitamin D2 (ergocalciferol) and vitamin D3 (cholecalciferol). Vitamin D3 is generally considered more effective at raising vitamin D levels in the blood. Thus, choosing a vitamin D3 supplement may offer an additional advantage in terms of bioavailability.
Who Needs Vitamin D Supplements?
Vitamin D deficiency is a widespread issue, affecting a significant portion of the global population. Several factors contribute to this deficiency, including inadequate sun exposure, dietary inadequacies, and certain medical conditions. Individuals at higher risk of vitamin D deficiency include:
-
Older adults: As people age, their skin’s ability to synthesize vitamin D from sunlight decreases, and their kidneys become less efficient at converting vitamin D to its active form.
-
People with limited sun exposure: Individuals who spend most of their time indoors, wear clothing that covers most of their skin, or live in regions with limited sunlight are at increased risk.
-
People with dark skin: Melanin, the pigment that gives skin its color, reduces the skin’s ability to produce vitamin D from sunlight.
-
People with certain medical conditions: Certain medical conditions, such as Crohn’s disease, celiac disease, and cystic fibrosis, can interfere with the absorption of vitamin D.
-
Obese individuals: Vitamin D is stored in fat tissue, making it less available for circulation in the body.
-
Infants: Breast milk may not provide sufficient vitamin D, and infants may require supplementation, especially if they are exclusively breastfed.
Health Implications of Vitamin D Deficiency
Vitamin D plays a critical role in various physiological processes, including calcium absorption, bone health, immune function, and muscle function. Vitamin D deficiency can have significant health consequences, including:
-
Rickets: In children, vitamin D deficiency can lead to rickets, a condition characterized by soft and weakened bones.
-
Osteomalacia: In adults, vitamin D deficiency can cause osteomalacia, a condition characterized by bone pain, muscle weakness, and an increased risk of fractures.
-
Osteoporosis: Vitamin D deficiency can contribute to osteoporosis, a condition characterized by decreased bone density and an increased risk of fractures.
-
Increased risk of infections: Vitamin D plays a crucial role in immune function, and deficiency can increase the risk of infections.
-
Muscle weakness and pain: Vitamin D deficiency can cause muscle weakness and pain.
-
Increased risk of cardiovascular disease: Some studies have suggested a link between vitamin D deficiency and an increased risk of cardiovascular disease, although more research is needed to confirm this association.
-
Increased risk of certain cancers: Some studies have suggested a link between vitamin D deficiency and an increased risk of certain cancers, such as colon cancer, breast cancer, and prostate cancer, although more research is needed to confirm these associations.
Optimal Vitamin D Levels and Supplementation Guidelines
The optimal vitamin D level is a subject of ongoing debate among healthcare professionals. However, most experts agree that a blood level of 20 nanograms per milliliter (ng/mL) or higher is generally considered sufficient for bone health and overall health. Some experts recommend a target level of 30-50 ng/mL for optimal health.
The recommended daily allowance (RDA) for vitamin D is 600 international units (IU) for adults aged 19-70 and 800 IU for adults over 70. However, many individuals may require higher doses to achieve optimal vitamin D levels, particularly those with risk factors for deficiency.
It is essential to consult with a healthcare professional to determine the appropriate vitamin D dosage based on individual needs and health status. A blood test can be performed to assess vitamin D levels and guide supplementation recommendations.
Food Sources of Vitamin D
While vitamin D supplements are often necessary to address deficiency, it is also possible to obtain vitamin D from dietary sources. However, relatively few foods are naturally rich in vitamin D. The best dietary sources of vitamin D include:
-
Fatty fish: Salmon, tuna, mackerel, and cod liver oil are excellent sources of vitamin D.
-
Fortified foods: Milk, yogurt, orange juice, and breakfast cereals are often fortified with vitamin D.
-
Egg yolks: Egg yolks contain small amounts of vitamin D.
-
Mushrooms: Some mushrooms, particularly those exposed to ultraviolet (UV) light, can produce vitamin D.
While dietary sources can contribute to vitamin D intake, it is often challenging to obtain sufficient amounts from food alone, particularly for individuals with limited sun exposure or certain medical conditions.
The Role of Sunlight in Vitamin D Production
Sunlight is the primary source of vitamin D for most people. When sunlight strikes the skin, it triggers the production of vitamin D3 (cholecalciferol). The amount of vitamin D produced depends on several factors, including:
-
Time of day: The sun’s rays are strongest during the midday hours, which is the most efficient time for vitamin D production.
-
Season: Vitamin D production is lower during the winter months, particularly in regions with limited sunlight.
-
Latitude: People living at higher latitudes (further from the equator) produce less vitamin D from sunlight.
-
Skin pigmentation: People with darker skin require more sun exposure to produce the same amount of vitamin D as people with lighter skin.
-
Age: As people age, their skin’s ability to produce vitamin D from sunlight decreases.
-
Sunscreen use: Sunscreen blocks the UVB rays that trigger vitamin D production.
While sunlight is an essential source of vitamin D, it is also important to protect the skin from excessive sun exposure to reduce the risk of skin cancer. Balancing sun exposure for vitamin D production with sun protection is crucial.
Potential Risks of Excessive Vitamin D Intake
While vitamin D deficiency is a common concern, it is also possible to take too much vitamin D. Excessive vitamin D intake can lead to hypercalcemia, a condition characterized by elevated levels of calcium in the blood. Symptoms of hypercalcemia can include nausea, vomiting, weakness, frequent urination, and kidney problems.
The upper tolerable intake level for vitamin D is 4,000 IU per day for adults. However, some individuals may tolerate higher doses under the supervision of a healthcare professional. It is important to avoid exceeding the recommended upper limit unless advised by a doctor.
The Importance of Consulting a Healthcare Professional
Given the complexities surrounding vitamin D status and supplementation, it is essential to consult with a healthcare professional to determine individual needs and ensure safe and effective supplementation. A doctor can assess vitamin D levels, evaluate risk factors for deficiency, and provide personalized recommendations for vitamin D intake. Self-treating with high doses of vitamin D without medical supervision can be risky and may lead to adverse health effects.
Conclusion
Optimizing vitamin D absorption involves strategic timing and dietary considerations. Taking vitamin D supplements with the largest meal of the day, particularly one containing healthy fats, can significantly enhance its bioavailability. While vitamin D supplements are often necessary to address deficiency, dietary sources and sunlight exposure also play important roles in maintaining adequate vitamin D levels. Consulting with a healthcare professional is crucial to determine individual needs and ensure safe and effective supplementation. Addressing vitamin D deficiency can have significant benefits for bone health, immune function, and overall well-being.
Frequently Asked Questions (FAQ)
1. What is the best time of day to take vitamin D for maximum absorption?
Experts recommend taking vitamin D with your largest meal of the day, especially if it contains fats. Vitamin D is a fat-soluble vitamin, so dietary fats help your body absorb it more efficiently. Studies suggest that taking vitamin D with a fat-containing meal can increase absorption compared to taking it on an empty stomach.
2. How much vitamin D should I take daily?
The recommended daily allowance (RDA) for vitamin D is 600 IU for adults aged 19-70 and 800 IU for adults over 70. However, individual needs may vary depending on factors such as age, skin color, sun exposure, and medical conditions. It is best to consult with a healthcare professional to determine the appropriate dosage for your specific needs. A blood test can help assess your vitamin D levels and guide supplementation recommendations.
3. What are the best food sources of vitamin D?
Relatively few foods are naturally rich in vitamin D. The best dietary sources include fatty fish such as salmon, tuna, and mackerel, as well as cod liver oil. Some foods are also fortified with vitamin D, including milk, yogurt, orange juice, and breakfast cereals. Egg yolks and certain mushrooms (particularly those exposed to UV light) contain small amounts of vitamin D.
4. Can I get enough vitamin D from sunlight alone?
Sunlight is a primary source of vitamin D, but the amount produced depends on several factors, including time of day, season, latitude, skin pigmentation, age, and sunscreen use. People living at higher latitudes, those with darker skin, and older adults may not produce enough vitamin D from sunlight alone, especially during the winter months. Sunscreen blocks the UVB rays that trigger vitamin D production. Supplementation may be necessary for individuals who cannot obtain sufficient vitamin D from sunlight.
5. What are the symptoms of vitamin D deficiency?
Symptoms of vitamin D deficiency can vary but may include fatigue, bone pain, muscle weakness, frequent infections, and mood changes. In children, severe vitamin D deficiency can lead to rickets, a condition characterized by soft and weakened bones. In adults, it can cause osteomalacia, leading to bone pain and muscle weakness. Vitamin D deficiency can also increase the risk of osteoporosis, fractures, and other health problems. If you suspect you may be deficient in vitamin D, it’s best to consult with a healthcare professional for testing and guidance.