A change in the dominant COVID-19 variant has brought with it a shift in the most commonly reported symptom: sore throat. Experts are now advising individuals experiencing sore throat, even without other classic COVID symptoms, to consider the possibility of infection and take appropriate precautions, including testing and isolation, to prevent further spread.
New COVID Variant Shifts Symptom Landscape: Sore Throat Now Predominant
The COVID-19 pandemic continues to evolve, and with it, the presentation of the illness. Public health officials and medical professionals are closely monitoring emerging variants and their associated symptoms. Currently, a notable trend has emerged: sore throat is now frequently reported as the primary symptom among individuals infected with newer strains of the virus. This shift necessitates increased vigilance and a revised understanding of how COVID-19 may initially manifest. This does not mean that previous symptoms such as fever, cough, fatigue, and loss of taste or smell have disappeared, but rather that sore throat is often the first and most prominent sign of infection in many cases.
“What we are seeing is that the constellation of symptoms seems to be a little bit different” says Dr. Thomas Russo, professor and chief of infectious disease at the University at Buffalo. He added that it is important to not rule out COVID-19 because you do not have all the classic symptoms.
The rise of sore throat as a leading symptom has implications for how individuals perceive and respond to potential infections. Previously, individuals might have dismissed a mild sore throat as a common cold or allergy. However, given the current prevalence of COVID-19, it is crucial to consider the possibility of infection, especially if the sore throat is accompanied by other symptoms such as fatigue, headache, or nasal congestion.
Why the Symptom Shift? Understanding Viral Evolution
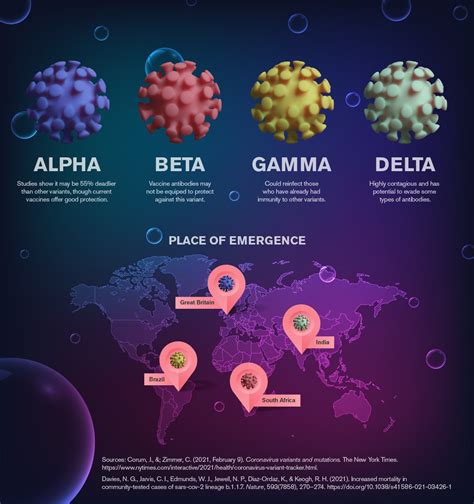
The evolution of viruses, including SARS-CoV-2, the virus responsible for COVID-19, is a continuous process. As the virus replicates and spreads, it undergoes mutations, leading to the emergence of new variants. These variants may possess altered characteristics, such as increased transmissibility, immune evasion, or changes in the severity and presentation of symptoms.
The precise reasons why sore throat has become a dominant symptom are multifaceted and likely related to the specific characteristics of the newer variants. Some experts suggest that the virus may be targeting different areas of the upper respiratory tract, leading to increased inflammation and irritation in the throat. Others speculate that changes in the virus’s spike protein, which it uses to enter cells, may affect the way it interacts with the respiratory system. Further research is needed to fully elucidate the underlying mechanisms driving this symptom shift.
Expert Recommendations: What You MUST Do
Given the evolving symptom landscape, health experts are emphasizing the importance of proactive measures to mitigate the spread of COVID-19. The following recommendations are crucial for individuals experiencing sore throat or other potential symptoms:
-
Consider the Possibility of COVID-19: Do not dismiss a sore throat as merely a common cold, especially if it is accompanied by other symptoms or if you have been in contact with someone who has tested positive for COVID-19. Maintain a heightened awareness of potential symptoms, even if they are mild.
-
Get Tested: If you experience a sore throat or other symptoms suggestive of COVID-19, it is essential to get tested as soon as possible. Rapid antigen tests, readily available at pharmacies and other locations, can provide quick results. However, if the initial rapid test is negative but symptoms persist, a PCR test, which is more sensitive, may be necessary.
-
Isolate Yourself: If you test positive for COVID-19, or if you suspect you may be infected, isolate yourself from others to prevent further spread. Follow the isolation guidelines recommended by your local health authorities. These guidelines typically involve staying home, avoiding contact with household members, and wearing a mask if you must be around others.
-
Seek Medical Advice: If you experience severe symptoms, such as difficulty breathing, persistent chest pain, or confusion, seek medical attention immediately. Early diagnosis and treatment can help prevent complications and improve outcomes. If you have underlying health conditions, consult with your doctor about potential treatment options, such as antiviral medications.
-
Practice Good Hygiene: Continue to practice good hygiene measures, such as frequent handwashing, covering your mouth and nose when you cough or sneeze, and avoiding touching your face. These measures can help prevent the spread of respiratory viruses, including COVID-19.
-
Stay Up-to-Date on Vaccinations: Vaccination remains the most effective way to protect yourself and others from severe illness, hospitalization, and death from COVID-19. Stay up-to-date on your vaccinations, including booster doses, as recommended by health authorities. Vaccines are designed to provide broad protection against different variants of the virus.
-
Ventilate Indoor Spaces: Improve ventilation in indoor spaces by opening windows and doors or using air purifiers. Proper ventilation can help reduce the concentration of virus particles in the air and lower the risk of transmission.
-
Monitor Symptoms: Closely monitor your symptoms. Even if your initial symptoms are mild, they can worsen over time. Keeping track of your symptoms will help you communicate effectively with healthcare providers and make informed decisions about your care.
The Importance of Testing and Accurate Diagnosis
Accurate and timely testing is crucial for managing the spread of COVID-19. Testing allows individuals to identify infections early, enabling them to isolate themselves and prevent transmission to others. It also provides valuable data for public health officials, who use it to track the spread of the virus, identify outbreaks, and implement appropriate control measures.
Both rapid antigen tests and PCR tests play important roles in COVID-19 testing. Rapid antigen tests offer the advantage of providing quick results, typically within 15-30 minutes. They are useful for screening individuals and identifying infections in real-time. However, rapid antigen tests are less sensitive than PCR tests, meaning they may be more likely to produce false negative results, especially in individuals with low viral loads or early in the course of infection.
PCR tests, on the other hand, are highly sensitive and can detect even small amounts of the virus. They are considered the gold standard for COVID-19 testing. However, PCR tests typically require laboratory processing, which can take longer to obtain results, sometimes up to several days.
The Role of Vaccination in Mitigating the Impact
Vaccination remains the cornerstone of efforts to mitigate the impact of COVID-19. COVID-19 vaccines have been shown to be highly effective in preventing severe illness, hospitalization, and death, even against newer variants of the virus.
The vaccines work by stimulating the immune system to produce antibodies and T cells that recognize and fight the virus. While vaccines may not always prevent infection entirely, they significantly reduce the risk of developing severe illness and complications.
Staying up-to-date on vaccinations, including booster doses, is crucial for maintaining optimal protection. The immunity provided by vaccines can wane over time, and booster doses help to boost the immune response and provide renewed protection.
Long-Term Implications and Future Strategies
The COVID-19 pandemic has had a profound impact on global health, economies, and societies. As the virus continues to evolve, it is essential to adapt strategies to effectively manage the pandemic and minimize its long-term consequences.
Ongoing research is crucial for understanding the virus, developing new vaccines and treatments, and improving diagnostic tools. Public health surveillance is essential for monitoring the spread of the virus, identifying new variants, and detecting outbreaks early.
In addition to medical interventions, it is important to address the social and economic factors that contribute to the spread of COVID-19. This includes addressing health disparities, promoting access to healthcare, and providing support for individuals and families affected by the pandemic.
The pandemic has highlighted the importance of global collaboration and solidarity. International cooperation is essential for sharing data, coordinating research efforts, and ensuring equitable access to vaccines and treatments.
The shift in the dominant symptom of COVID-19 underscores the need for continued vigilance and adaptation. By staying informed, practicing good hygiene, and following expert recommendations, individuals can play a crucial role in mitigating the spread of the virus and protecting themselves and others.
The pandemic is not over, and it is important to remain vigilant and proactive. By working together, we can navigate the challenges ahead and build a healthier and more resilient future.
Mental Health Considerations
The ongoing COVID-19 pandemic has not only impacted physical health but has also taken a significant toll on mental well-being. The constant barrage of information, the fear of infection, the isolation of lockdowns, and the economic uncertainties have contributed to increased rates of anxiety, depression, and other mental health conditions.
It is important to prioritize mental health and seek support when needed. Talking to friends, family, or a mental health professional can help individuals cope with stress and anxiety. Engaging in activities that promote well-being, such as exercise, meditation, and spending time in nature, can also be beneficial.
Employers, schools, and communities can play a role in promoting mental health by providing resources and support services. Creating a culture of openness and acceptance around mental health can help reduce stigma and encourage individuals to seek help when they need it.
Addressing Misinformation and Promoting Accurate Information
The COVID-19 pandemic has been accompanied by a surge of misinformation and disinformation, which can have serious consequences for public health. False or misleading information can lead individuals to make poor decisions about their health, such as refusing to get vaccinated or using unproven treatments.
It is important to be critical of the information you consume and to rely on credible sources, such as public health agencies, medical professionals, and scientific organizations. Be wary of information that is sensationalized, lacks evidence, or comes from unreliable sources.
Fact-checking websites can help you verify the accuracy of information. Sharing accurate information with your friends and family can help counter the spread of misinformation.
The Impact on Children and Education
The COVID-19 pandemic has had a significant impact on children and education. School closures, remote learning, and social isolation have disrupted children’s learning and development.
Many children have experienced learning loss during the pandemic. They may have fallen behind in their studies or missed out on important social and emotional learning opportunities.
It is important to provide support for children to help them catch up academically and address any social and emotional challenges they may be facing. This includes providing tutoring, counseling, and other support services.
Schools can play a role in promoting children’s well-being by creating a safe and supportive learning environment. Parents can support their children by encouraging them to stay engaged in learning and providing them with emotional support.
FAQ: New COVID Variant and Sore Throat
-
Q: Is sore throat always a sign of COVID-19?
A: No, a sore throat can be caused by many things, including common colds, allergies, and strep throat. However, given the current prevalence of COVID-19, especially with newer variants, it’s essential to consider COVID-19 as a possibility if you experience a sore throat, even without other classic COVID symptoms. Testing is recommended to confirm or rule out the infection. As Dr. Russo states, do not rule out COVID-19 because you do not have all the classic symptoms.
-
Q: What should I do if I have a sore throat but test negative for COVID-19 with a rapid test?
A: If you have a sore throat and test negative on a rapid antigen test, but your symptoms persist, it’s recommended to get a PCR test. Rapid tests are less sensitive and can sometimes produce false negatives, especially early in the infection. Isolate yourself until you receive the PCR test results to prevent potential spread. Consider seeking advice from a healthcare professional, especially if you have underlying health conditions.
-
Q: Are there other symptoms I should watch out for besides a sore throat?
A: While sore throat is now a commonly reported initial symptom, other symptoms of COVID-19 can include fever, cough, fatigue, headache, muscle aches, loss of taste or smell, nasal congestion, and gastrointestinal issues like nausea, vomiting, or diarrhea. Symptoms can vary in intensity and combination, so it’s important to be vigilant and monitor your overall health.
-
Q: How effective are the current COVID-19 vaccines against the new variants?
A: Current COVID-19 vaccines are still effective in preventing severe illness, hospitalization, and death, even against newer variants. However, their effectiveness against preventing infection may be somewhat reduced. Booster doses are recommended to enhance protection and maintain immunity over time. Staying up-to-date with your vaccinations is the best way to protect yourself and others.
-
Q: If I’ve had COVID-19 before, can I get it again with the new variant?
A: Yes, it is possible to get COVID-19 again, even if you’ve had it before. Natural immunity from a previous infection may not provide complete protection against new variants. Vaccination, even after a previous infection, can provide additional protection and reduce the risk of reinfection and severe illness.
The Economic Repercussions of Ongoing Infections
Beyond the direct health impacts, the continued prevalence of COVID-19 infections, even with milder symptoms, carries significant economic repercussions. Frequent absences from work due to illness or isolation disrupt productivity and can strain businesses, particularly small enterprises. The healthcare system also faces ongoing costs associated with testing, treatment, and long-term care for those experiencing long COVID. The economic burden underscores the importance of preventative measures, such as vaccination and responsible behavior, to minimize the overall impact of the pandemic.
The Importance of Public Health Infrastructure
The COVID-19 pandemic has highlighted the critical role of a robust public health infrastructure. Public health agencies are responsible for monitoring disease trends, conducting surveillance, implementing control measures, and communicating information to the public. Investing in public health infrastructure is essential for preparing for and responding to future pandemics and other health emergencies. This includes strengthening laboratory capacity, training public health professionals, and improving data collection and analysis systems.
The Ethical Considerations of Public Health Measures
Public health measures, such as mask mandates and vaccine requirements, often involve ethical considerations. Balancing the need to protect public health with individual liberties can be challenging. It is important to have open and transparent discussions about the ethical implications of public health measures and to ensure that they are implemented in a fair and equitable manner. Respecting individual autonomy while safeguarding the well-being of the community requires careful consideration and thoughtful decision-making.
Navigating the “New Normal”
As the COVID-19 pandemic continues to evolve, societies are adapting to a “new normal.” This involves incorporating preventative measures into daily life, such as practicing good hygiene, staying home when sick, and getting vaccinated. It also requires adapting workplaces, schools, and other settings to minimize the risk of transmission. The “new normal” is not a return to the pre-pandemic world, but rather a new way of living that balances the need to protect public health with the desire to resume normal activities. It requires ongoing flexibility, adaptation, and a commitment to collective responsibility.
The Role of Technology in Pandemic Management
Technology has played a crucial role in managing the COVID-19 pandemic. Telemedicine has enabled patients to access healthcare remotely, reducing the risk of exposure to the virus. Contact tracing apps have helped to identify and isolate individuals who have been exposed to the virus. Data analytics tools have been used to track the spread of the virus and inform public health decision-making. Continued innovation in technology will be essential for improving pandemic preparedness and response in the future.
Addressing Health Disparities
The COVID-19 pandemic has disproportionately affected certain populations, including racial and ethnic minorities, low-income communities, and individuals with disabilities. These disparities are often rooted in systemic inequities in access to healthcare, housing, and other resources. Addressing health disparities is essential for achieving health equity and ensuring that everyone has the opportunity to live a healthy life. This requires addressing the underlying social and economic factors that contribute to health disparities, as well as implementing targeted interventions to improve the health of vulnerable populations.
The Future of Pandemic Preparedness
The COVID-19 pandemic has served as a wake-up call, highlighting the importance of pandemic preparedness. Investing in research, strengthening public health infrastructure, and promoting global collaboration are essential for preparing for future pandemics. Developing new vaccines and treatments, improving diagnostic tools, and strengthening surveillance systems are crucial steps. Learning from the lessons of the COVID-19 pandemic will help to ensure that the world is better prepared to respond to future health emergencies.
The Mental Health Impacts on Healthcare Workers
The COVID-19 pandemic has placed immense strain on healthcare workers, who have been on the front lines of the response. Long hours, exposure to the virus, and the emotional toll of caring for critically ill patients have contributed to increased rates of burnout, anxiety, and depression among healthcare workers. Providing support for healthcare workers is essential for their well-being and for ensuring that they are able to continue providing high-quality care. This includes providing access to mental health services, offering flexible work arrangements, and creating a supportive work environment.
The Long-Term Effects of COVID-19 (Long COVID)
Many individuals who have recovered from COVID-19 continue to experience long-term symptoms, a condition known as long COVID. These symptoms can include fatigue, brain fog, shortness of breath, and other health problems. The long-term effects of COVID-19 can significantly impact individuals’ quality of life and ability to work. More research is needed to understand the causes of long COVID and to develop effective treatments. Providing support for individuals with long COVID is essential for helping them manage their symptoms and improve their quality of life.
The Role of Community Organizations
Community organizations play a vital role in responding to the COVID-19 pandemic. They can provide support for vulnerable populations, disseminate information, and promote vaccination. Community organizations are often trusted sources of information and can reach individuals who may not be reached by traditional public health channels. Partnering with community organizations is essential for ensuring an equitable and effective pandemic response.
The Importance of Clear and Consistent Communication
Clear and consistent communication is essential for building public trust and promoting adherence to public health recommendations. Public health agencies should communicate information in a clear, concise, and accessible manner. They should also be transparent about what is known and unknown about the virus and the pandemic. Building trust and fostering open communication are crucial for encouraging individuals to take actions that protect their health and the health of their communities.
The COVID-19 pandemic continues to present challenges, but by staying informed, practicing good hygiene, and following expert recommendations, individuals can play a crucial role in mitigating the spread of the virus and protecting themselves and others. The shift in the dominant symptom underscores the need for ongoing vigilance and adaptation. By working together, we can navigate the challenges ahead and build a healthier and more resilient future.