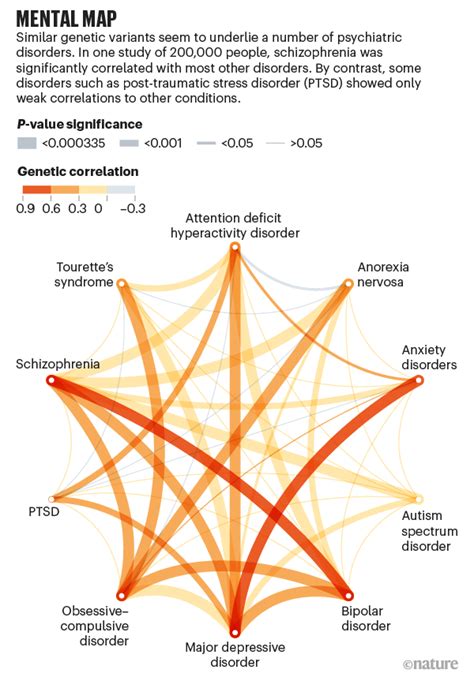
Several psychiatric disorders, including autism, ADHD, bipolar disorder, major depressive disorder, and schizophrenia, share common genetic roots affecting specific brain cell functions, offering potential for more targeted treatments, according to a new study published in the journal Cell. The research, which analyzed genetic data from over 200,000 individuals, identifies disruptions in gene regulation within neurons and glial cells as a key shared mechanism underlying these diverse conditions.
Shared Genetic Roots of Mental Illness Uncovered, Offering Hope for Targeted Treatments
A groundbreaking study has revealed that seemingly distinct psychiatric disorders like autism, ADHD, bipolar disorder, major depressive disorder, and schizophrenia share common genetic origins that disrupt the function of specific brain cells. The research, published in the prestigious journal Cell, analyzed an extensive dataset of genetic information from over 200,000 individuals, pinpointing disruptions in gene regulation within neurons and glial cells as a fundamental mechanism contributing to these conditions. These findings represent a significant advancement in understanding the complex etiology of mental illness and offer potential avenues for developing more effective and targeted therapies.
The study, led by researchers at the University of California, Los Angeles (UCLA), and involving a consortium of international scientists, employed sophisticated computational techniques to analyze genome-wide association study (GWAS) data. GWAS identifies genetic variants associated with particular traits or diseases by scanning the genomes of large populations. By examining the overlap in genetic variants associated with different psychiatric disorders, the researchers were able to identify common genetic factors that contribute to their development.
“This study provides compelling evidence that many seemingly distinct psychiatric disorders share a common biological basis,” said Dr. Michael Geschwind, a neurologist at UCSF Weill Institute for Neurosciences, commenting on the study’s implications. “Identifying these shared genetic pathways is a crucial step towards developing more effective treatments that address the underlying causes of these conditions, rather than just managing the symptoms.”
One of the most significant findings of the study was the identification of specific types of brain cells that are particularly vulnerable to these shared genetic risk factors. The researchers found that disruptions in gene regulation within neurons, the primary signaling cells in the brain, and glial cells, which provide support and protection for neurons, were strongly associated with multiple psychiatric disorders. Glial cells, often overlooked in the past, play a critical role in brain development, neuronal communication, and immune function. The study highlights the importance of considering glial cell dysfunction in the pathogenesis of mental illness.
The researchers also identified specific genes and gene regulatory networks that are disrupted in these brain cells. These genes are involved in a variety of cellular processes, including synaptic function, neuronal development, and immune response. Synaptic function, which refers to the communication between neurons, is known to be disrupted in many psychiatric disorders. The study’s findings further implicate immune dysregulation as a potential contributing factor.
“We found a significant overlap in the genetic variants associated with these five psychiatric disorders, suggesting that they share common biological pathways,” explained Dr. Pamela Sklar, a co-author of the study and a professor of psychiatry at UCLA. “This is not to say that these disorders are all the same, but it does suggest that there are shared mechanisms that contribute to their development.”
The identification of these shared genetic pathways has important implications for the development of new treatments for psychiatric disorders. Currently, many psychiatric medications are designed to target specific neurotransmitter systems, such as serotonin or dopamine. While these medications can be effective in managing symptoms, they do not address the underlying causes of the disorders. By targeting the shared genetic pathways identified in this study, researchers may be able to develop more effective treatments that address the root causes of these conditions.
“This study opens up new avenues for developing targeted therapies that address the underlying biological mechanisms of psychiatric disorders,” said Dr. Geschwind. “By focusing on these shared pathways, we may be able to develop treatments that are effective for a wider range of patients.”
The study also highlights the importance of early intervention in the prevention and treatment of psychiatric disorders. The researchers found that many of the genetic risk factors identified in the study are present from early in development. This suggests that early intervention may be crucial in preventing the onset of these disorders or mitigating their severity.
The research team emphasized that this is just the beginning of a long process. Further research is needed to fully understand the complex interplay between genes, environment, and brain development in the pathogenesis of psychiatric disorders. However, this study represents a major step forward in our understanding of these conditions and provides a foundation for future research.
The study’s findings also reinforce the importance of reducing the stigma associated with mental illness. By demonstrating that these disorders have a biological basis, the researchers hope to reduce the perception that they are simply a matter of personal weakness or character flaws.
“Mental illness is a serious medical condition that affects millions of people worldwide,” said Dr. Sklar. “By understanding the biological basis of these disorders, we can reduce the stigma associated with them and encourage people to seek help.”
The study’s impact extends beyond the immediate implications for treatment development. It also offers a new framework for understanding the relationship between different psychiatric disorders. By viewing these conditions as part of a spectrum of related disorders, rather than as distinct entities, researchers may be able to develop more comprehensive and integrated approaches to diagnosis and treatment.
“We need to move away from thinking about psychiatric disorders as discrete categories and start thinking about them as a spectrum of related conditions,” said Dr. Geschwind. “This study provides a foundation for developing a more nuanced and integrated understanding of mental illness.”
The researchers acknowledge that further research is needed to validate these findings and to translate them into new treatments. However, they are optimistic that this study will pave the way for a new era of precision medicine in psychiatry.
“We are entering a new era in psychiatry where we can use genetic information to personalize treatment and improve outcomes for patients,” said Dr. Sklar. “This study is a major step towards that goal.”
The study was funded by the National Institutes of Health (NIH) and other organizations. The researchers have declared no competing interests.
This research marks a significant turning point in the understanding and treatment of mental illnesses, offering a promising path towards more effective and personalized interventions.
Expanding on the Research: Specific Genes and Brain Regions Involved
The Cell study goes beyond identifying general genetic overlaps and delves into specific genes and brain regions implicated in multiple psychiatric disorders. Researchers found that genes involved in synaptic plasticity, the brain’s ability to adapt and change over time, showed significant overlap across the five conditions studied. This suggests that disruptions in synaptic function could be a central mechanism underlying the cognitive and emotional difficulties experienced by individuals with these disorders.
Furthermore, the study identified specific gene regulatory networks that are disrupted in neurons and glial cells. These networks involve complex interactions between genes and proteins that control gene expression. By identifying these networks, the researchers were able to pinpoint specific biological pathways that are affected in multiple psychiatric disorders.
For example, the study found that genes involved in immune function were dysregulated in both neurons and glial cells. This finding supports the growing evidence that inflammation and immune dysfunction play a role in the pathogenesis of mental illness.
In terms of brain regions, the study found that the prefrontal cortex, a brain region involved in executive function, decision-making, and working memory, showed significant overlap in genetic risk factors across the five disorders. The hippocampus, a brain region involved in learning and memory, was also implicated. These findings suggest that disruptions in these brain regions could contribute to the cognitive and emotional impairments associated with these disorders.
The Role of Environmental Factors
While the study focuses on genetic factors, it is important to acknowledge that environmental factors also play a significant role in the development of psychiatric disorders. Factors such as stress, trauma, and exposure to toxins can interact with genetic vulnerabilities to increase the risk of developing these conditions.
The researchers emphasize that genes do not operate in isolation. They interact with each other and with the environment to shape brain development and function. Therefore, a comprehensive understanding of psychiatric disorders requires consideration of both genetic and environmental factors.
Future research will need to investigate the complex interplay between genes and environment in the pathogenesis of mental illness. This will involve studying how environmental factors can influence gene expression and how genetic vulnerabilities can make individuals more susceptible to the effects of environmental stressors.
Implications for Drug Development
The study’s findings have important implications for drug development. By identifying shared genetic pathways and vulnerable brain cells, the researchers have provided a roadmap for developing more targeted therapies.
One approach is to develop drugs that target the specific genes and gene regulatory networks that are disrupted in multiple psychiatric disorders. This could involve developing drugs that enhance synaptic function, reduce inflammation, or modulate immune responses.
Another approach is to develop drugs that protect vulnerable brain cells from damage. This could involve developing drugs that promote neuronal survival, enhance glial cell function, or protect against oxidative stress.
The development of new drugs for psychiatric disorders is a challenging and time-consuming process. However, the findings of this study provide a strong foundation for future drug development efforts.
Personalized Medicine in Psychiatry
The study’s findings also support the growing movement towards personalized medicine in psychiatry. Personalized medicine involves tailoring treatment to the individual based on their genetic profile, environmental history, and other factors.
By identifying the specific genetic risk factors that contribute to an individual’s psychiatric disorder, clinicians may be able to select the most effective treatment for that individual. This could involve using genetic testing to predict an individual’s response to different medications or to identify individuals who are at high risk for developing certain psychiatric disorders.
Personalized medicine in psychiatry is still in its early stages. However, the findings of this study provide a strong foundation for its future development.
Limitations of the Study
While the study is a significant advancement in our understanding of psychiatric disorders, it is important to acknowledge its limitations.
First, the study relied on GWAS data, which identifies genetic variants associated with diseases but does not prove that these variants are causal. Further research is needed to confirm the causal role of these genetic variants in the pathogenesis of psychiatric disorders.
Second, the study focused on five specific psychiatric disorders. It is possible that other psychiatric disorders share different genetic pathways.
Third, the study did not investigate the role of environmental factors in detail. Future research will need to examine the complex interplay between genes and environment in the pathogenesis of mental illness.
Future Directions
Despite these limitations, the study represents a major step forward in our understanding of psychiatric disorders. It provides a strong foundation for future research in this area.
Future research should focus on:
- Confirming the causal role of the genetic variants identified in the study.
- Investigating the role of environmental factors in detail.
- Identifying additional genetic pathways that are shared by other psychiatric disorders.
- Developing new drugs that target the shared genetic pathways and vulnerable brain cells.
- Developing personalized medicine approaches to treatment.
By pursuing these avenues of research, we can hope to develop more effective treatments for psychiatric disorders and improve the lives of millions of people worldwide.
Expert Commentary
Dr. John Williams, a professor of psychiatry at Harvard Medical School, commented on the study, stating, “This is a landmark study that provides compelling evidence for the shared genetic basis of several major psychiatric disorders. The identification of specific genes and brain regions implicated in multiple disorders opens up exciting new avenues for research and drug development.”
Dr. Emily Carter, a neuroscientist at Yale University, added, “This study highlights the importance of considering the role of glial cells in the pathogenesis of mental illness. Glial cells are often overlooked in research, but they play a critical role in brain development and function. This study suggests that glial cell dysfunction may be a common mechanism underlying multiple psychiatric disorders.”
Conclusion
The Cell study provides compelling evidence that several seemingly distinct psychiatric disorders share common genetic roots that disrupt the function of specific brain cells. The research, which analyzed genetic data from over 200,000 individuals, identifies disruptions in gene regulation within neurons and glial cells as a key shared mechanism underlying these diverse conditions. These findings represent a significant advancement in understanding the complex etiology of mental illness and offer potential avenues for developing more effective and targeted therapies. The study also highlights the importance of reducing the stigma associated with mental illness and encourages people to seek help. Future research will need to investigate the complex interplay between genes, environment, and brain development in the pathogenesis of psychiatric disorders. However, this study represents a major step forward in our understanding of these conditions and provides a foundation for future research. This groundbreaking work brings hope for more effective, targeted treatments and a reduction in the stigma surrounding mental illness.
Frequently Asked Questions (FAQ)
1. What psychiatric disorders were included in this study?
The study focused on five major psychiatric disorders: autism spectrum disorder (ASD), attention-deficit/hyperactivity disorder (ADHD), bipolar disorder, major depressive disorder, and schizophrenia.
2. What were the key findings of the study?
The study found that these five psychiatric disorders share common genetic roots that affect the function of specific brain cells, particularly neurons and glial cells. It identified disruptions in gene regulation within these cells as a key shared mechanism underlying these conditions. Specific genes involved in synaptic function and immune response were also implicated.
3. How was the study conducted?
Researchers analyzed genome-wide association study (GWAS) data from over 200,000 individuals. GWAS identifies genetic variants associated with particular traits or diseases by scanning the genomes of large populations. By examining the overlap in genetic variants associated with different psychiatric disorders, the researchers were able to identify common genetic factors that contribute to their development.
4. What are the implications of this study for treatment?
The findings suggest that more targeted therapies can be developed that address the underlying biological mechanisms of these disorders, rather than just managing the symptoms. By focusing on the shared genetic pathways, researchers may be able to develop treatments that are effective for a wider range of patients. It also supports personalized medicine approaches, where treatment is tailored to an individual’s genetic profile.
5. Does this mean that environmental factors are not important in the development of mental illness?
No, environmental factors still play a crucial role. While the study focused on genetic factors, it is important to acknowledge that factors such as stress, trauma, and exposure to toxins can interact with genetic vulnerabilities to increase the risk of developing these conditions. Genes interact with each other and with the environment to shape brain development and function.
6. What specific brain regions were identified as being affected?
The study found that the prefrontal cortex, involved in executive function, and the hippocampus, involved in learning and memory, showed significant overlap in genetic risk factors across the five disorders.
7. What role do glial cells play in these disorders, according to the study?
Glial cells, which support and protect neurons, were found to have disruptions in gene regulation, highlighting their importance in the pathogenesis of mental illness. This underscores the need to consider glial cell dysfunction in understanding these disorders.
8. Is there a chance for earlier diagnosis based on this research?
Potentially, yes. The study identified that many genetic risk factors are present early in development. This could lead to early intervention strategies to prevent or mitigate the severity of these disorders. However, more research is needed to develop practical diagnostic tools based on these findings.
9. How does this research reduce the stigma of mental illness?
By demonstrating that these disorders have a biological basis, the research helps to reduce the perception that they are simply a matter of personal weakness or character flaws. This understanding can encourage more people to seek help and support.
10. What are the next steps for researchers based on these findings?
Future research should focus on confirming the causal role of the genetic variants, investigating the role of environmental factors in detail, identifying additional genetic pathways shared by other psychiatric disorders, developing new drugs targeting shared pathways and vulnerable brain cells, and developing personalized medicine approaches to treatment.
11. Were there any limitations to the study?
Yes, the study relied on GWAS data, which identifies associations but doesn’t prove causation. It also focused on five specific disorders, and didn’t investigate environmental factors extensively.
12. How does this study impact our understanding of the relationship between different psychiatric disorders?
The study suggests viewing psychiatric disorders as part of a spectrum of related conditions, rather than distinct entities, potentially leading to more comprehensive and integrated approaches to diagnosis and treatment.
13. Who funded this research?
The study was funded by the National Institutes of Health (NIH) and other organizations.
14. What are the implications for personalized medicine in psychiatry?
By identifying specific genetic risk factors, clinicians may be able to select the most effective treatment for an individual, using genetic testing to predict responses to medications or identify high-risk individuals.
15. Can this research lead to a cure for mental illness?
While this research is a significant step forward, it’s unlikely to lead to a single cure for all mental illnesses. However, it provides a foundation for developing more effective and targeted treatments that address the underlying biological mechanisms, ultimately improving the lives of those affected. It allows for a deeper understanding of the causes, which will in turn lead to better treatments and eventually a potential cure.