A medical office is grappling with the fallout of a romantic relationship between two employees, which has reportedly created a hostile work environment and led to the departure of one of the individuals, potentially necessitating the hiring of a new doctor to maintain adequate staffing and patient care.
The situation, detailed in a query submitted to Slate’s “Dear Prudence” advice column, involves a doctor who pursued a romantic relationship with a staff member, creating significant workplace tension after the relationship ended. According to the advice seeker, who identifies as working in the same office, the doctor initiated the relationship by “aggressively pursuing” the staff member, despite initial reluctance. The fallout has now resulted in the staff member resigning and the remaining staff are considering seeking new employment themselves, leaving the practice potentially short-staffed and seeking a replacement physician.
The original letter writer, deeply concerned about the ethical and professional implications of the situation, sought advice on how to navigate the tense atmosphere and address the broader issue of workplace conduct. The core problem stems from a power dynamic inherent in the relationship, exacerbated by the doctor’s perceived abuse of authority in initiating and pursuing the relationship. This has subsequently led to a poisoned work environment affecting the morale and stability of the entire office.
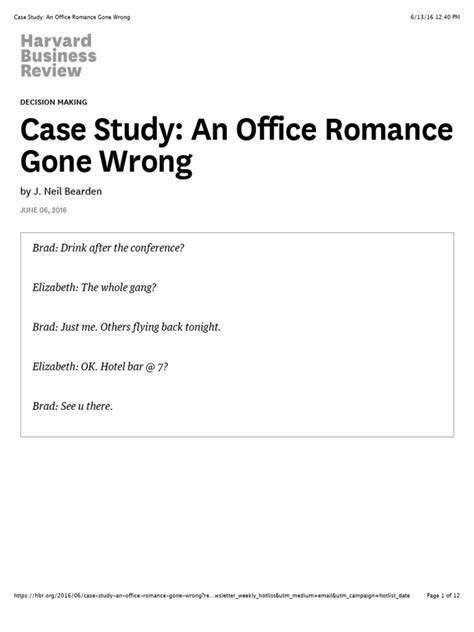
The letter writer explained, “Soooo, I work in a small medical office where one of the doctors (we’ll call him Dr. Hubris) asked out a cute guy who works in the office (we’ll call him Dave). Dave politely declined, but Dr. Hubris kept pushing. Dave eventually gave in, and they dated for about six months. Then Dave broke up with him, and Dr. Hubris did not take it well.”
The advice column response highlighted the severe ethical lapse and potential legal ramifications of the doctor’s behavior. Prudence (Emily Yoffe) emphasized the imbalance of power and the potential for coercion, suggesting that the doctor’s actions could be construed as harassment. The response underscored the importance of maintaining professional boundaries in the workplace, especially within hierarchical structures. The advice focused on the importance of the other employees taking steps to protect themselves and ensure a safe and respectful work environment.
The collapse of the relationship and the subsequent hostile work environment have created a ripple effect, impacting not only the individuals directly involved but also the overall functionality and stability of the medical practice. The remaining staff members are reportedly demoralized and considering leaving their positions, potentially leading to a critical staffing shortage. This disruption could compromise the quality of patient care and place additional strain on the remaining personnel.
The medical office is now confronted with several pressing issues: addressing the immediate need to restore a positive work environment, managing the potential fallout from the staff member’s departure, and strategically planning for the possibility of recruiting a new doctor. These challenges require a multifaceted approach, including implementing clear workplace policies, providing sensitivity training, and potentially seeking legal counsel to ensure compliance with employment laws and regulations.
The situation underscores the importance of robust workplace policies that explicitly prohibit romantic relationships between individuals in positions of power and their subordinates. Such policies are designed to prevent conflicts of interest, protect employees from potential harassment, and maintain a professional and respectful work environment. Moreover, the incident highlights the need for effective mechanisms for reporting and addressing workplace misconduct, ensuring that employees feel safe and empowered to speak out against inappropriate behavior.
The ramifications of this “office romance gone wrong” extend beyond the immediate impact on the individuals involved and the medical practice. It also raises broader questions about ethical conduct in professional settings, the importance of power dynamics, and the potential consequences of blurring personal and professional boundaries. This incident serves as a cautionary tale for employers and employees alike, emphasizing the need to prioritize professionalism, respect, and ethical behavior in the workplace.
The potential departure of more staff members exacerbates the existing challenges, potentially leading to longer wait times for patients, reduced availability of appointments, and increased workload for the remaining employees. The medical practice may need to consider offering incentives to retain existing staff, such as increased salaries, improved benefits, or opportunities for professional development.
Furthermore, the medical office may need to engage in damage control to mitigate any negative publicity resulting from the incident. This could involve communicating openly and transparently with patients, reassuring them that the practice is committed to providing high-quality care, and addressing any concerns or questions they may have.
The recruitment of a new doctor presents its own set of challenges. The medical practice will need to conduct a thorough search to identify qualified candidates who not only possess the necessary skills and experience but also align with the practice’s values and culture. The recruitment process should also include measures to ensure that the new doctor is aware of the practice’s policies on workplace conduct and is committed to maintaining a professional and respectful work environment.
In addition to addressing the immediate staffing needs, the medical practice should also consider implementing long-term strategies to prevent similar incidents from occurring in the future. This could involve conducting regular training sessions on workplace ethics, harassment prevention, and conflict resolution. It could also involve establishing a clear and confidential process for reporting and investigating complaints of misconduct.
The incident serves as a reminder that workplace relationships, especially those involving power imbalances, can have significant and far-reaching consequences. Employers have a responsibility to create a safe and respectful work environment for all employees, and employees have a responsibility to conduct themselves professionally and ethically. By prioritizing these values, organizations can minimize the risk of workplace conflicts and ensure that all employees are able to thrive.
The “Dear Prudence” response also touched on the legal implications of Dr. Hubris’s behavior, suggesting that Dave may have grounds for a legal claim of harassment, depending on the specific circumstances and applicable state laws. The advice columnist encouraged the letter writer to consult with an employment attorney to explore potential legal options and protect their own rights.
The situation also highlights the importance of bystander intervention. The letter writer, as a colleague of both Dr. Hubris and Dave, has a responsibility to speak out against the inappropriate behavior and support the victim. While it may be difficult or uncomfortable to confront a superior, failing to do so can perpetuate a culture of silence and allow the misconduct to continue.
The medical practice should also consider implementing a formal employee assistance program (EAP) to provide confidential counseling and support services to employees who may be experiencing stress, anxiety, or other emotional difficulties. An EAP can help employees cope with the challenges of the workplace and address any personal issues that may be affecting their performance or well-being.
The situation in the medical office is a complex and multifaceted one, with no easy solutions. However, by taking proactive steps to address the immediate challenges, implement long-term prevention strategies, and prioritize the well-being of its employees, the practice can begin to rebuild trust, restore a positive work environment, and ensure that it is able to continue providing high-quality care to its patients.
The fallout from the failed relationship continues to reverberate through the office, with staff morale plummeting and productivity declining. The remaining employees are reportedly feeling anxious, stressed, and uncertain about the future of the practice. Some are actively seeking new employment opportunities, while others are hesitant to leave due to concerns about job security or a lack of alternative options.
The medical practice may need to consider offering temporary incentives to retain existing staff, such as increased salaries, bonuses, or additional time off. These incentives could help to alleviate some of the financial stress and emotional burden that the employees are experiencing.
In addition, the practice should consider implementing a formal communication plan to keep employees informed about the progress of the situation and any changes that may be occurring. Regular updates and open dialogue can help to reduce anxiety and uncertainty and foster a sense of transparency and trust.
The situation also raises questions about the role of leadership in creating and maintaining a positive work environment. The medical practice’s leadership team should take responsibility for addressing the root causes of the problem and implementing strategies to prevent similar incidents from occurring in the future. This may involve conducting a thorough review of the practice’s policies and procedures, providing training on workplace ethics and harassment prevention, and fostering a culture of open communication and accountability.
The incident serves as a reminder that workplace relationships can have a significant impact on the overall culture and productivity of an organization. Employers have a responsibility to create a safe and respectful environment for all employees, and employees have a responsibility to conduct themselves professionally and ethically. By prioritizing these values, organizations can minimize the risk of workplace conflicts and ensure that all employees are able to thrive.
The medical practice may also want to consider engaging an external consultant to help facilitate a dialogue among the staff and address the underlying issues that are contributing to the toxic work environment. A neutral third party can provide a safe space for employees to express their concerns and work collaboratively to find solutions.
The consultant could also help the practice develop a comprehensive plan for improving workplace culture and preventing future incidents of misconduct. This plan could include specific goals, timelines, and accountability measures.
The incident also highlights the importance of having a clear and well-defined process for handling complaints of harassment or discrimination. Employees should know how to report such complaints, and they should be confident that their concerns will be taken seriously and investigated thoroughly.
The medical practice should also ensure that all employees are aware of their rights under applicable employment laws. This includes the right to be free from harassment and discrimination, the right to a safe and healthy work environment, and the right to report violations of the law without fear of retaliation.
The situation in the medical office is a complex and challenging one, but it is not insurmountable. By taking proactive steps to address the immediate issues, implement long-term prevention strategies, and prioritize the well-being of its employees, the practice can begin to rebuild trust, restore a positive work environment, and ensure that it is able to continue providing high-quality care to its patients.
The situation has forced the medical practice to confront uncomfortable truths about its workplace culture and the potential for abuse of power. The incident serves as a wake-up call for the practice’s leadership team, who must now take decisive action to address the underlying issues and create a more equitable and respectful environment for all employees.
The practice may also want to consider implementing a mentorship program to provide support and guidance to junior employees. A mentor can serve as a trusted advisor and role model, helping employees navigate the challenges of the workplace and develop their professional skills.
The mentorship program could also help to foster a sense of community and connection among employees, which can be particularly important in a small medical office where relationships are often close-knit.
In addition to the mentorship program, the medical practice could also consider establishing an employee resource group (ERG) to provide a forum for employees to connect with others who share similar backgrounds or interests. An ERG can help to promote diversity and inclusion within the workplace and create a sense of belonging for all employees.
The ERG could also serve as a resource for the practice’s leadership team, providing feedback on policies and practices that may be affecting employees from underrepresented groups.
The situation in the medical office underscores the importance of ongoing training and development for all employees. Training should cover topics such as workplace ethics, harassment prevention, conflict resolution, and cultural sensitivity.
The training should be interactive and engaging, and it should be tailored to the specific needs of the medical practice. The practice should also ensure that all employees have access to ongoing learning opportunities, such as conferences, workshops, and online courses.
The incident also highlights the importance of creating a culture of accountability within the medical practice. All employees should be held accountable for their actions, and those who violate the practice’s policies or ethical standards should be subject to appropriate disciplinary action.
The practice should also have a clear and transparent process for investigating allegations of misconduct and taking corrective action. This process should be fair and impartial, and it should protect the rights of both the accuser and the accused.
The situation in the medical office is a complex and challenging one, but it is also an opportunity for the practice to learn and grow. By taking proactive steps to address the immediate issues, implement long-term prevention strategies, and prioritize the well-being of its employees, the practice can emerge stronger and more resilient than before.
The incident has also raised concerns about the potential impact on the medical practice’s reputation. The practice may need to take steps to manage its public image and reassure patients that it is committed to providing high-quality care.
This could involve communicating with patients directly, updating the practice’s website and social media profiles, and engaging with the local community. The practice should also be prepared to respond to any negative publicity that may arise.
The medical practice should also consider seeking advice from a public relations professional to help manage its reputation and communicate effectively with its stakeholders.
The situation in the medical office is a reminder that workplace relationships can be complex and challenging, and that they can have significant consequences for both individuals and organizations. Employers have a responsibility to create a safe and respectful environment for all employees, and employees have a responsibility to conduct themselves professionally and ethically. By prioritizing these values, organizations can minimize the risk of workplace conflicts and ensure that all employees are able to thrive.
Frequently Asked Questions (FAQ)
-
What exactly happened in the medical office?
A doctor in the office pursued a romantic relationship with a staff member (Dave) who initially declined. The doctor persisted, and they dated for approximately six months. After Dave ended the relationship, the doctor reportedly reacted poorly, creating a hostile work environment. This situation has led to Dave’s resignation and is prompting other staff members to consider leaving, potentially leaving the office short-staffed. As reported by the letter writer, “Dave politely declined, but Dr. Hubris kept pushing. Dave eventually gave in, and they dated for about six months. Then Dave broke up with him, and Dr. Hubris did not take it well.”
-
What was the advice given in the “Dear Prudence” column about this situation?
The “Dear Prudence” advice emphasized the ethical lapse and potential legal ramifications of the doctor’s behavior. The advice focused on the imbalance of power and the potential for coercion, suggesting that the doctor’s actions could be construed as harassment. The response underscored the importance of maintaining professional boundaries in the workplace, especially within hierarchical structures. The advice focused on the importance of the other employees taking steps to protect themselves and ensure a safe and respectful work environment and consulting with an employment attorney.
-
Why is the power dynamic between the doctor and staff member a significant issue in this situation?
The power dynamic is significant because the doctor’s position of authority could be seen as coercive. This inherent power imbalance can make it difficult for the staff member to freely consent to a relationship without fear of professional repercussions or retaliation. The doctor’s “aggressively pursuing” behavior exacerbated this issue, raising concerns about potential harassment and abuse of authority.
-
What are the potential consequences for the medical office as a result of this situation?
The potential consequences include:
- Staff Shortage: The resignation of the staff member and the potential departure of other employees could lead to a critical staffing shortage, affecting patient care and increasing workload for remaining staff.
- Hostile Work Environment: The tense atmosphere could negatively impact employee morale and productivity.
- Reputational Damage: The incident could damage the medical practice’s reputation, leading to loss of patients.
- Legal Issues: The doctor’s behavior could result in legal action for harassment or creating a hostile work environment.
- Increased Costs: The need to recruit and train new staff, as well as potential legal fees, could increase the practice’s expenses.
-
What steps can the medical office take to address this situation and prevent similar incidents in the future?
The medical office can take several steps:
- Implement Clear Workplace Policies: Establish policies that explicitly prohibit romantic relationships between individuals in positions of power and their subordinates.
- Provide Sensitivity Training: Conduct training on workplace ethics, harassment prevention, and conflict resolution for all employees.
- Establish Reporting Mechanisms: Create a clear and confidential process for reporting and investigating complaints of misconduct.
- Offer Employee Assistance Program (EAP): Provide confidential counseling and support services to employees.
- Engage Legal Counsel: Consult with an employment attorney to ensure compliance with laws and regulations.
- Promote Open Communication: Foster a culture of open communication and accountability, where employees feel safe speaking out against inappropriate behavior.
- Leadership Accountability: The leadership team should take responsibility for addressing the root causes of the problem and implementing strategies to prevent similar incidents from occurring in the future.
- Mentorship Program: Implement a mentorship program to provide support and guidance to junior employees.
- Employee Resource Group: Establish an employee resource group (ERG) to provide a forum for employees to connect with others who share similar backgrounds or interests.
- Review and Update Policies: Regularly review and update workplace policies to ensure they are effective and compliant with applicable laws.
- Bystander Intervention Training: Train employees to recognize and safely intervene in situations involving potential harassment or misconduct.
- Formal Apology: A formal apology from the doctor could help to rebuild trust and restore a positive work environment.
- Independent Investigation: An independent investigation into the doctor’s behavior can help to determine the extent of the misconduct and identify any necessary corrective actions.
- Performance Evaluation: The doctor’s performance evaluation should reflect the seriousness of the misconduct and outline specific expectations for future behavior.
-
What are the potential legal ramifications for the doctor involved? The doctor could face legal repercussions depending on the specific circumstances and applicable state laws. These could include:
-
Harassment Claims: Dave may have grounds for a harassment claim if the doctor’s behavior created a hostile work environment. This includes unwelcome advances, offensive remarks, or other conduct that interferes with Dave’s ability to perform his job.
-
Abuse of Power: The doctor’s position of authority could be seen as an abuse of power, particularly if Dave felt pressured to enter into the relationship due to fear of professional consequences.
-
Violation of Workplace Policies: If the medical practice has policies prohibiting romantic relationships between supervisors and subordinates, the doctor may have violated those policies.
-
Disciplinary Action: The medical practice may take disciplinary action against the doctor, up to and including termination of employment.
It’s important for Dave to consult with an employment attorney to explore his legal options and protect his rights.
- How can the remaining staff members cope with the tense atmosphere?
Remaining staff members can cope with the tense atmosphere by:
-
Documenting Incidents: Keeping a record of any inappropriate behavior or comments they witness.
-
Seeking Support: Talking to a trusted friend, family member, or therapist about their feelings.
-
Setting Boundaries: Establishing clear boundaries with the doctor and avoiding unnecessary interactions.
-
Consulting with HR: If the medical practice has an HR department, they can consult with HR professionals about their concerns.
-
Exploring Legal Options: Consulting with an employment attorney to understand their legal rights and options.
-
Practicing Self-Care: Engaging in activities that help them relax and de-stress, such as exercise, meditation, or spending time with loved ones.
-
Supporting Each Other: Providing support and encouragement to their colleagues who are also struggling with the situation.
- How can the medical practice ensure patient care is not affected during this difficult time?
The medical practice can ensure patient care is not affected during this difficult time by:
-
Prioritizing Patient Needs: Focusing on providing high-quality care to all patients.
-
Maintaining Open Communication: Keeping patients informed about any changes to the practice’s operations.
-
Offering Flexible Scheduling: Providing flexible scheduling options to accommodate patients’ needs.
-
Ensuring Adequate Staffing: Hiring temporary staff or reallocating existing staff to ensure adequate coverage.
-
Monitoring Patient Satisfaction: Monitoring patient satisfaction levels and addressing any concerns promptly.
-
Expressing Gratitude: Thanking patients for their understanding and support during this challenging time.
-
Transparency: Openly communicating with patients about the situation in the office to reassure them.
- What is the role of bystander intervention in this situation? Bystander intervention plays a crucial role in preventing and addressing workplace misconduct. In this situation, colleagues of both the doctor and the staff member have a responsibility to speak out against inappropriate behavior and support the victim.
-
Recognizing Inappropriate Behavior: Bystanders must be able to identify situations where harassment, discrimination, or abuse of power may be occurring. This includes recognizing subtle cues, such as uncomfortable body language or changes in behavior.
-
Taking Action: Once inappropriate behavior is recognized, bystanders can take several actions to intervene. These include:
- Direct Intervention: Directly confronting the harasser and telling them to stop.
- Indirect Intervention: Supporting the victim by offering assistance, listening to their concerns, and validating their experience.
- Reporting the Incident: Reporting the incident to HR or other appropriate authorities.
-
Creating a Culture of Accountability: Bystander intervention helps to create a culture of accountability in the workplace, where employees are held responsible for their actions and where harassment and discrimination are not tolerated.
-
Promoting a Safe and Respectful Environment: By intervening in situations involving misconduct, bystanders can help to promote a safe and respectful environment for all employees.
-
Training: Providing bystander intervention training can empower employees to take action when they witness inappropriate behavior. This training should cover topics such as recognizing harassment, safely intervening, and reporting incidents.
- What are some long-term strategies the medical practice can implement to foster a healthier workplace culture?
To foster a healthier workplace culture in the long term, the medical practice can implement the following strategies:
-
Leadership Commitment: The practice’s leadership must be fully committed to creating a culture of respect, inclusivity, and ethical behavior. This commitment should be communicated clearly and consistently to all employees.
-
Regular Training: Provide regular training on topics such as workplace ethics, harassment prevention, conflict resolution, and cultural sensitivity. This training should be interactive and engaging, and it should be tailored to the specific needs of the medical practice.
-
Open Communication: Foster a culture of open communication, where employees feel comfortable expressing their concerns and providing feedback. This can be achieved through regular staff meetings, anonymous feedback surveys, and one-on-one conversations with supervisors.
-
Employee Recognition: Recognize and reward employees for their contributions to the practice and for demonstrating ethical behavior. This can be done through formal recognition programs, informal appreciation, and opportunities for professional development.
-
Work-Life Balance: Promote work-life balance by providing flexible work arrangements, encouraging employees to take time off, and offering wellness programs.
-
Diversity and Inclusion: Create a diverse and inclusive workplace where all employees feel valued and respected. This can be achieved through targeted recruitment efforts, diversity and inclusion training, and employee resource groups.
-
Conflict Resolution: Establish a clear and effective process for resolving conflicts between employees. This process should be fair and impartial, and it should protect the rights of all parties involved.
-
Continuous Improvement: Regularly evaluate the practice’s workplace culture and identify areas for improvement. This can be done through employee surveys, focus groups, and external assessments.
By implementing these strategies, the medical practice can create a healthier and more supportive workplace culture, which will benefit employees, patients, and the practice as a whole.









