Sun exposure in the late morning to midday hours proves most effective for maximizing vitamin D absorption, according to health experts, due to the sun’s UVB rays being at their peak intensity during this period. This optimal timing allows for efficient vitamin D synthesis in the skin, critical for bone health, immune function, and overall well-being.
The sun’s UVB rays are essential for vitamin D production, converting a cholesterol-based precursor in the skin into vitamin D3, the active form of the vitamin. “The best time to get vitamin D from the sun is between 10 a.m. and 3 p.m.,” says Dr. Michael Holick, a leading expert in vitamin D research and professor of medicine at Boston University. “This is when the UVB rays are most intense.” During these hours, the sun is higher in the sky, meaning UVB rays have a shorter distance to travel through the atmosphere, resulting in greater intensity at the Earth’s surface.
Beyond just timing, the amount of skin exposed and skin pigmentation also significantly influence vitamin D synthesis. Light-skinned individuals typically require less time in the sun compared to those with darker skin. “People with darker skin need more sun exposure to produce the same amount of vitamin D as people with lighter skin,” explains Dr. Holick. This is because melanin, the pigment responsible for skin color, acts as a natural sunscreen, reducing the penetration of UVB rays.
Experts recommend that individuals with lighter skin expose their arms and legs to the sun for about 10-15 minutes during midday, while those with darker skin may require 30 minutes to several hours to achieve adequate vitamin D production. However, these are general guidelines, and individual needs can vary based on factors like age, health conditions, and geographical location. It’s crucial to balance sun exposure with the risk of sunburn and skin damage, emphasizing the importance of sun protection measures like sunscreen after the initial period of vitamin D synthesis.
The use of sunscreen, while essential for protecting against skin cancer, can significantly reduce vitamin D production. Sunscreens with a Sun Protection Factor (SPF) of 30 or higher can block up to 97% of UVB rays. Therefore, it’s recommended to get some sun exposure without sunscreen before applying it, particularly during the optimal window for vitamin D synthesis.
Vitamin D deficiency is a widespread concern, affecting a significant portion of the global population. Insufficient vitamin D levels have been linked to various health problems, including weakened bones (osteoporosis), increased risk of infections, and potential associations with chronic diseases like heart disease, diabetes, and certain cancers. Symptoms of vitamin D deficiency can be subtle and may include fatigue, bone pain, muscle weakness, and mood changes.
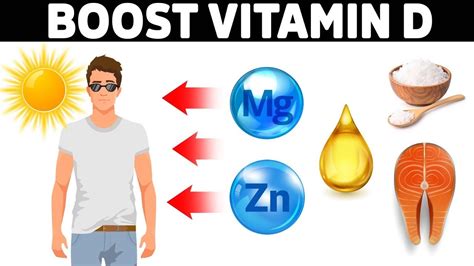
Dietary sources of vitamin D are limited. Fatty fish like salmon, tuna, and mackerel are good sources, as are egg yolks and fortified foods like milk and cereals. However, it can be challenging to obtain sufficient vitamin D from diet alone, making sun exposure and supplementation important strategies for maintaining adequate levels.
Vitamin D supplements are available in two forms: vitamin D2 (ergocalciferol) and vitamin D3 (cholecalciferol). Vitamin D3 is generally considered more effective at raising blood levels of vitamin D. The recommended daily intake of vitamin D varies depending on age and individual needs, but most adults are advised to consume at least 600 International Units (IU) per day. Individuals with vitamin D deficiency may require higher doses, as determined by a healthcare professional.
The geographical location also plays a crucial role in vitamin D synthesis. People living in northern latitudes, where sunlight is weaker during the winter months, are at higher risk of vitamin D deficiency. During these times, supplementation and dietary sources become even more important.
Medical conditions that affect vitamin D absorption, such as Crohn’s disease, celiac disease, and cystic fibrosis, can also increase the risk of deficiency. Individuals with these conditions may require higher doses of vitamin D supplementation under the guidance of a healthcare provider.
Regular blood tests can help determine vitamin D levels and identify any deficiencies. A healthcare provider can recommend appropriate strategies for maintaining optimal vitamin D levels based on individual needs and risk factors.
In conclusion, maximizing vitamin D absorption involves a combination of strategic sun exposure, a balanced diet, and, when necessary, supplementation. Understanding the optimal timing for sun exposure, considering individual factors like skin pigmentation and sunscreen use, and being aware of potential risk factors for vitamin D deficiency are all essential for maintaining optimal health.
Expanding on the Importance of Vitamin D
Vitamin D, often dubbed the “sunshine vitamin,” transcends its traditional association with bone health, emerging as a crucial player in a wide array of physiological processes. Its influence spans from immune modulation to cardiovascular function, highlighting its significance in maintaining overall well-being. A deeper understanding of vitamin D’s multifaceted roles underscores the importance of optimizing its levels through strategic lifestyle choices and, when necessary, supplementation.
Beyond Bones: Vitamin D’s Systemic Impact
While its role in calcium absorption and bone mineralization is well-established, vitamin D’s influence extends far beyond skeletal health. Receptors for vitamin D are found throughout the body, suggesting its involvement in numerous cellular functions.
- Immune Modulation: Vitamin D plays a critical role in regulating the immune system. It helps to modulate both innate and adaptive immune responses, contributing to immune homeostasis. Studies have shown that vitamin D deficiency is associated with an increased susceptibility to infections, including respiratory infections like influenza and COVID-19. Vitamin D enhances the function of immune cells, such as macrophages and T cells, enabling them to effectively combat pathogens.
- Cardiovascular Health: Emerging evidence suggests a link between vitamin D deficiency and an increased risk of cardiovascular disease. Vitamin D may help regulate blood pressure, improve endothelial function, and reduce inflammation, all of which are important for maintaining cardiovascular health. Some studies have shown that vitamin D supplementation may improve cardiovascular outcomes in individuals with deficiency.
- Cancer Prevention: Research has explored the potential role of vitamin D in cancer prevention. Vitamin D may help regulate cell growth and differentiation, promote apoptosis (programmed cell death) in cancer cells, and inhibit angiogenesis (the formation of new blood vessels that feed tumors). While more research is needed, some studies have suggested that higher vitamin D levels may be associated with a reduced risk of certain cancers, including colorectal, breast, and prostate cancer.
- Mental Health: Vitamin D may also play a role in mental health. Studies have linked vitamin D deficiency to an increased risk of depression, seasonal affective disorder (SAD), and other mood disorders. Vitamin D may influence the production and regulation of neurotransmitters, such as serotonin and dopamine, which are important for mood regulation.
- Muscle Function: Vitamin D is essential for maintaining muscle strength and function. Vitamin D deficiency can lead to muscle weakness, fatigue, and an increased risk of falls, particularly in older adults. Vitamin D supplementation has been shown to improve muscle strength and balance in individuals with deficiency.
- Diabetes Management: Some studies suggest that vitamin D may play a role in glucose metabolism and insulin sensitivity. Vitamin D deficiency has been associated with an increased risk of type 2 diabetes, and vitamin D supplementation may improve glycemic control in individuals with diabetes.
Optimizing Vitamin D Levels: A Multifaceted Approach
Achieving and maintaining optimal vitamin D levels requires a comprehensive approach that considers individual factors, lifestyle choices, and, when necessary, supplementation.
- Strategic Sun Exposure: As highlighted in the initial summary, strategic sun exposure remains a primary method for stimulating vitamin D production. Midday sun exposure, between 10 a.m. and 3 p.m., maximizes UVB ray exposure, facilitating efficient vitamin D synthesis. However, it’s crucial to balance sun exposure with the risk of sunburn and skin damage. Starting with short periods of sun exposure and gradually increasing the duration can help minimize the risk of sunburn. Regular monitoring of skin for any changes is also recommended.
- Dietary Intake: Incorporating vitamin D-rich foods into the diet can contribute to overall vitamin D levels. Fatty fish, such as salmon, tuna, and mackerel, are excellent sources of vitamin D. Egg yolks, fortified milk, and fortified cereals can also provide vitamin D. However, dietary sources alone may not be sufficient to meet daily requirements, particularly for individuals with limited sun exposure or increased vitamin D needs.
- Supplementation: Vitamin D supplements are a convenient and effective way to ensure adequate vitamin D intake, especially during winter months or for individuals with risk factors for deficiency. Vitamin D3 (cholecalciferol) is generally considered more effective than vitamin D2 (ergocalciferol) at raising blood levels of vitamin D. The recommended daily intake of vitamin D varies depending on age and individual needs, but most adults are advised to consume at least 600 IU per day. Individuals with vitamin D deficiency may require higher doses, as determined by a healthcare professional.
- Regular Monitoring: Regular blood tests to check vitamin D levels can help identify any deficiencies and guide appropriate intervention strategies. A healthcare provider can interpret test results and recommend personalized strategies for optimizing vitamin D levels based on individual needs and risk factors. The 25-hydroxyvitamin D (25(OH)D) blood test is the standard method for assessing vitamin D status.
Factors Influencing Vitamin D Status
Several factors can influence an individual’s vitamin D status, including:
- Skin Pigmentation: Melanin, the pigment responsible for skin color, absorbs UVB rays, reducing vitamin D synthesis. Individuals with darker skin require more sun exposure to produce the same amount of vitamin D as those with lighter skin.
- Age: As we age, the skin’s ability to produce vitamin D decreases. Older adults are also more likely to have reduced sun exposure and impaired vitamin D absorption, increasing their risk of deficiency.
- Geographical Location: People living in northern latitudes, where sunlight is weaker during the winter months, are at higher risk of vitamin D deficiency.
- Sunscreen Use: Sunscreen blocks UVB rays, reducing vitamin D synthesis. While sunscreen is essential for protecting against skin cancer, it can also contribute to vitamin D deficiency.
- Medical Conditions: Certain medical conditions, such as Crohn’s disease, celiac disease, cystic fibrosis, and kidney disease, can impair vitamin D absorption or metabolism, increasing the risk of deficiency.
- Obesity: Vitamin D is stored in fat tissue, making it less available in the circulation. Obese individuals are more likely to have lower vitamin D levels.
- Medications: Certain medications, such as corticosteroids, anticonvulsants, and some HIV medications, can interfere with vitamin D metabolism, increasing the risk of deficiency.
Addressing Vitamin D Deficiency: A Personalized Approach
Addressing vitamin D deficiency requires a personalized approach that considers individual risk factors, lifestyle choices, and underlying medical conditions. A healthcare provider can assess an individual’s vitamin D status, identify any contributing factors, and recommend appropriate strategies for optimizing vitamin D levels. These strategies may include:
- Increased Sun Exposure: Safe and strategic sun exposure can help stimulate vitamin D production. However, it’s important to avoid sunburn and protect the skin from excessive sun damage.
- Dietary Modifications: Incorporating vitamin D-rich foods into the diet can contribute to overall vitamin D levels.
- Supplementation: Vitamin D supplements are an effective way to raise vitamin D levels, particularly for individuals with deficiency or risk factors for deficiency. The dosage and duration of supplementation should be determined by a healthcare provider.
- Treatment of Underlying Medical Conditions: Addressing any underlying medical conditions that may be contributing to vitamin D deficiency is essential.
- Lifestyle Modifications: Making lifestyle changes, such as increasing physical activity and maintaining a healthy weight, can also improve vitamin D status.
Conclusion: Vitamin D – A Cornerstone of Health
Vitamin D is a vital nutrient that plays a crucial role in maintaining overall health and well-being. Its influence extends far beyond bone health, impacting immune function, cardiovascular health, mental health, and more. Optimizing vitamin D levels through strategic sun exposure, a balanced diet, and, when necessary, supplementation is essential for preventing deficiency and promoting optimal health. Regular monitoring of vitamin D levels and personalized interventions based on individual needs and risk factors are key to ensuring adequate vitamin D status and reaping its numerous health benefits. The information shared by experts highlights the crucial need for understanding the ideal time for sun exposure and using the knowledge to improve vitamin D levels.
Frequently Asked Questions (FAQ)
-
What is the best time of day to get vitamin D from the sun?
The best time to get vitamin D from the sun is typically between 10 a.m. and 3 p.m. This is when the sun’s UVB rays are at their peak intensity, allowing for efficient vitamin D synthesis in the skin. “The best time to get vitamin D from the sun is between 10 a.m. and 3 p.m.,” says Dr. Michael Holick. “This is when the UVB rays are most intense.”
-
How much sun exposure is needed to produce adequate vitamin D?
The amount of sun exposure needed varies depending on skin pigmentation, age, geographical location, and other factors. Generally, light-skinned individuals may need about 10-15 minutes of sun exposure on their arms and legs during midday, while those with darker skin may require 30 minutes to several hours. It’s important to avoid sunburn and protect the skin from excessive sun damage.
-
Does sunscreen block vitamin D production?
Yes, sunscreen can significantly reduce vitamin D production. Sunscreens with an SPF of 30 or higher can block up to 97% of UVB rays. It’s recommended to get some sun exposure without sunscreen before applying it, particularly during the optimal window for vitamin D synthesis.
-
What are the symptoms of vitamin D deficiency?
Symptoms of vitamin D deficiency can be subtle and may include fatigue, bone pain, muscle weakness, and mood changes. In severe cases, vitamin D deficiency can lead to rickets in children and osteomalacia in adults, both characterized by weakened bones.
-
What are good dietary sources of vitamin D?
Good dietary sources of vitamin D include fatty fish like salmon, tuna, and mackerel, as well as egg yolks and fortified foods like milk and cereals. However, it can be challenging to obtain sufficient vitamin D from diet alone, making sun exposure and supplementation important strategies for maintaining adequate levels.
Additional FAQs:
-
Can I get enough vitamin D from tanning beds?
While some tanning beds emit UVB rays, which can stimulate vitamin D production, the risks associated with tanning bed use, such as skin cancer, outweigh the potential benefits. It’s generally not recommended to use tanning beds for vitamin D synthesis.
-
Are vitamin D supplements safe?
Vitamin D supplements are generally safe when taken at recommended doses. However, excessive intake of vitamin D can lead to toxicity, characterized by symptoms such as nausea, vomiting, weakness, and kidney problems. It’s important to follow the recommended dosage guidelines and consult with a healthcare provider before taking high doses of vitamin D.
-
How do I know if I am vitamin D deficient?
The only way to know for sure if you are vitamin D deficient is to have a blood test performed by your healthcare provider. The 25-hydroxyvitamin D (25(OH)D) blood test is the standard method for assessing vitamin D status.
-
Is vitamin D2 or vitamin D3 better?
Vitamin D3 (cholecalciferol) is generally considered more effective than vitamin D2 (ergocalciferol) at raising blood levels of vitamin D. Therefore, vitamin D3 is the preferred form for supplementation.
-
What should I do if I am diagnosed with vitamin D deficiency?
If you are diagnosed with vitamin D deficiency, your healthcare provider will recommend a treatment plan based on the severity of your deficiency and your individual needs. This may involve a combination of increased sun exposure, dietary modifications, and vitamin D supplementation. It’s important to follow your healthcare provider’s recommendations and monitor your vitamin D levels regularly to ensure that your treatment is effective.
Expanding further, it is worth noting some other factors that can affect the production of vitamin D:
- Cloud cover and pollution: Cloud cover and air pollution can reduce the amount of UVB rays that reach the Earth’s surface, which can decrease vitamin D production.
- Latitude: People living at higher latitudes are at greater risk of vitamin D deficiency because the sun’s UVB rays are weaker in these areas, especially during the winter months.
- Time of year: Vitamin D production is typically lower during the winter months due to the reduced intensity of UVB rays and decreased sun exposure.
- Clothing: Wearing clothing that covers most of the skin can significantly reduce vitamin D production.
The optimal level of Vitamin D in the blood can be determined using a blood test and discussed with your doctor. There is no “one size fits all” approach to the issue of ensuring sufficient Vitamin D levels, but a combination of awareness of the factors that lead to vitamin D deficiencies coupled with appropriate action based on the advice of your doctor is a good foundation for a path to better health.









